Why Is it important for surgeons who are not dealing with gender-related procedures to be attuned to the evolving field of gender identity and sexual orientation?
Concepts of gender identity and sexual orientation are not new; they find benevolent mention in many ancient Greek and Roman writings dating back over 2000 years. Periods of varying degrees of persecution have since followed. As of late, society has become more open to embracing the non-binary gender distribution and differences in sexual orientation. Gender is typically assigned at birth in a binary manner: male or female based on chromosomal and/or physical anatomical attributes. As life unfolds, many individuals are at ease and identify with the gender they were assigned at birth (cisgender); others recognize traits of both genders within themselves and wish to express this in form of non-binary gender identity, or come to the realization altogether that their birth gender is entirely mismatched with their current identity (transgender). Since this process of self-realization is frequently arduous and painful, gender identity can be quite emotionally charged and failure to accurately acknowledge it might cause significant emotional distress, negatively impact patient-physician interactions and ultimately cause adverse medical outcomes [1]. Sexual orientation, on the other hand, refers to the gender choice one makes when seeking a romantic/sexual partner. Gay and lesbian sexual orientation refers to individuals who have sex or are romantically involved with a partner of the same gender. Bisexual orientation refers to an individual who “falls in love with a person, regardless of their gender.” Respecting our patients’ identities and choices is crucial for an effective patient-physician relationship based on trust and a lack of fear of discrimination.
How can a neurosurgeon and their staff create an environment that is welcoming to all patients regardless of their gender identity and sexual orientation?
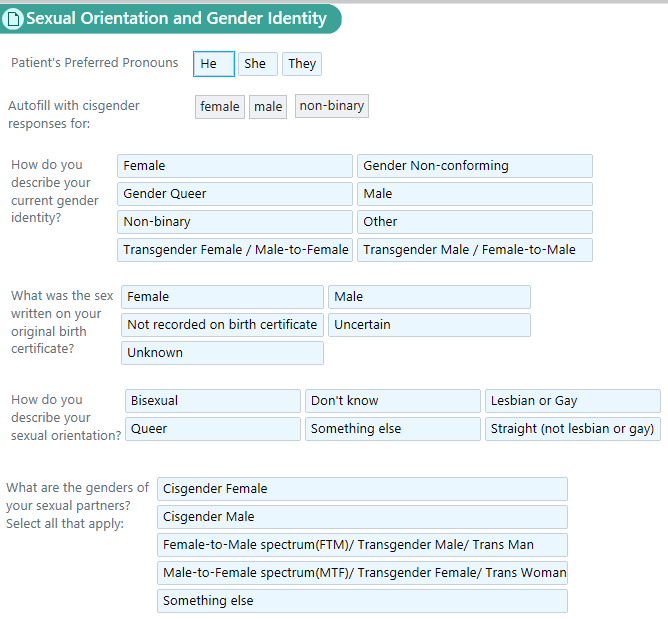
All staff members with direct patient contact should be trained on matters relating to sensitivity towards gender non-conforming patients and members of the LGBTQ+ community [2]. Changing simple terms on patient intake forms may create a more welcoming environment and allow for a stronger up-front professional relationship. Examples include using terms such as “relationship status” instead of “marital status,” or including options like “partnered.” When asking about a patient’s “partner/spouse” ask about their “gender”. This might make patients feel more at ease than having to disclose their sexual orientation. Similarly, when asking about gender, consider adding “gender assigned at birth” and “current gender”. Most impactful, however, is the attitude each of us has toward this topic. If one feels “phobic” or dismissive about it, the patient will feel it. This is also true for the interaction we have with our staff and colleagues. It is also important to note that although patients may use terms like “gay”, “dyke” or “queer” themselves, those can have a derogatory connotation especially if they are ascribed uninvited to a patient by a healthcare professional. Therefore, it is advisable to use language that is not offensive, like “sexual partner of the same or opposite gender”
Being Cisgender and heterosexual are associated with a lower risk of negative health and life outcomes. Why is that?
Individuals who don’t fall within the cisgender and heterosexual categories are referred to as LGBTQ+. They often feel and/or are discriminated against, marginalized and ultimately receive suboptimal care leading to inferior clinical outcomes [3]. LGBTQ+ youths are more likely to consider suicide [4]. Discrimination is widely experienced by LGBTQ+ patients across all aspects of health care, especially among racial/ethnic minorities, and more than one in six LGBTQ+ adults reports avoiding health care due to anticipated discrimination [5] Recognizing that training the next generation of physicians requires promoting excellence in LGBTQ+ health as well as advocacy for the unique sets of needs that patients in the LGBTQ+ community have, the American Medical Association Foundation has partnered with the Icahn School of Medicine at Mount Sinai to underwrite a pilot fellowship program in LGBTQ+ healthcare delivery [6].
In your pioneer role as fellowship director of one of the two such programs in the U.S., what do you think are the most important goals of this educational initiative?
The fellowship strives to provide a comprehensive educational experience encompassing all aspects of LGBTQ+ focused medical care including primary care, primary and secondary prevention of disease, gender-affirming endocrine and surgical care as well as mental health and addiction. An additional goal is to help set national standards for post-graduate education in LGBTQ+ medicine in collaboration with the American Medical Association.
References
1. https://pubmed.ncbi.nlm.nih.gov/31509158/; https://pubmed.ncbi.nlm.nih.gov/32192577/; https://pubmed.ncbi.nlm.nih.gov/17463371/; https://pubmed.ncbi.nlm.nih.gov/20516373/
2. https://glma.org/_data/n_0001/resources/live/GLMA%20guidelines%202006%20FINAL.pdf
3. https://www.lgbtqiahealtheducation.org/wp-content/uploads/LGBTHealthDisparitiesMar2016.pdf
4. https://www.cdc.gov/healthyyouth/disparities/health-disparities-among-lgbtq-youth.htm; https://pubmed.ncbi.nlm.nih.gov/21783042/
5. https://pubmed.ncbi.nlm.nih.gov/31659745/
6. https://health.mountsinai.org/blog/mount-sinai-creates-lgbtq-medical-fellowship-that-will-serve-as-a-national-model-of-care/