The views expressed in this article are those of the author and do not reflect the official policy of the Department of Army/Navy/Air Force, Department of Defense or U.S. Government.
Peripheral nerve trauma has long been recognized by military physicians as a consequence of combat where the soldier’s head and internal organs are protected by armor, but the extremities remain exposed. Homer even describes what appears to be a brachial plexus injury in The Iliad, nearly 3,000 years ago. He writes: “… [Hector] hit him just where the collar-bone divides the neck from the chest, a very deadly place, and broke the sinew of his arm so that his wrist was less, and the bow dropped from his hand as he fell forward on his knees.”

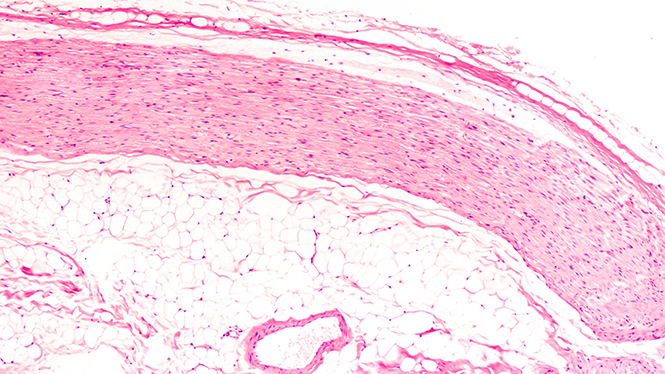
Over the last 3,000 years, combat has certainly changed, with a Trojan horse now referring to a method of electronic warfare rather than the legendary wooden decoy, however soldiers continue to experience peripheral nerve trauma from extremities that are not protected by modern body armor. While deployed I evaluated two patients injured in a 107mm Katyusha rocket attack who each sustained fragmentation injuries to the extremities (Figure 1 and 2). One patient had a large entrance wound in the right buttock with the fragment passing just posterior and lateral to the sciatic nerve, which could be palpated through the wound itself. The nerve was inspected and neurolysed, with only minor bruising present, and the patient maintained full function of the lower extremity. The other patient was injured in the same rocket strike, holding up his arms in a blocking fashion and had several fragments lodged in his upper extremities, the largest of which was removed from his forearm. Thankfully no nerve injuries were identified.

With troop levels in the Middle East decreasing, the incidence of wartime peripheral nerve injury in forward deployed troops is also decreasing, but peripheral nerve injury remains common in civilian extremity trauma. According to Padovono et. al (2020), nerve injuries are present in 2.6% of upper extremity trauma cases, but only 40% of nerve injuries are diagnosed by the time the patient is discharged from the hospital. More concerning, 12.2% of brachial plexus injuries are not diagnosed until more than 1 year has passed since the trauma itself. While in many cases of peripheral nerve trauma there is little to do in the acute phase (outside of clean, sharp lacerations), identification of the nerve injury and proper localization is paramount. After nerve injury, the newly denervated muscle atrophies, and unless reinnervated (prior to 18-24 months), tends to undergo irreversible atrophy and fibrosis. Repaired nerves can grow approximately 1mm/day, but in many cases must grow over long distances to reach the denervated muscle, ultimately meaning early identification and localization is key for any attempt at repair and/or reconstruction.
The options for primary repair, nerve transfers and secondary reconstruction have expanded greatly over recent years, bringing ever more strategies and techniques for functional recovery to the patient with a debilitating peripheral nerve injury. In 2017, Maldonado et al wrote the paper titled “Five Operations That Give the Best Results after Brachial Plexus Injury,” describing Leechavengvongs procedure, Oberlin transfer, free functioning muscle (gracilis) transfer, radial nerve tendon transfers and C5-6 nerve grafting for obstetrical birth palsy as surgical options with good, reproducible results in these often challenging situations. Simultaneously, advances in prosthetics are leading to lighter and more functional devices that give patients with unrecoverable injuries a useful extremity once again. Further advances in reconstruction and pain control after nerve injury have been described by Dr. Gregory Dumanian, who has helped to study and popularize targeted muscle reinnervation, leading to a fundamental shift in post-amputation pain management.
The care of patients with peripheral nerve injuries is often complex, and requires multidisciplinary evaluation and treatment to address chances of recovery, reconstruction options, and management of associated pain. These patients are often best served by a multidisciplinary clinic that includes neurosurgery, plastic surgery, orthopedic hand surgery, neurology, PMR, pain, therapists and perhaps most important, a dedicated coordinator to streamline the process for both patients and providers. This arrangement allows for detailed discussions of complex management and reconstruction strategies that are often required in these cases.
Unfortunately for the Greeks, the famous physicians Machaon and Podalirius didn’t have a multidisciplinary team to help them treat nerve injuries after hand-to-hand combat. But then again, they only had to deal with paper (parchment) charts, not the modern day EMR.
References
- Maldonado AA, Bishop AT, Spinner RJ, Shin AY. Five Operations That Give the Best Results after Brachial Plexus Injury. Plast Reconstr Surg. 2017 Sep;140(3):545-556. doi: 10.1097/PRS.0000000000003620. PMID: 28574948.
- Padovano WM, Dengler J, Patterson MM, Yee A, Snyder-Warwick AK, Wood MD, Moore AM, Mackinnon SE. Incidence of Nerve Injury After Extremity Trauma in the United States. Hand (N Y). 2020 Oct 21:1558944720963895. doi: 10.1177/1558944720963895. Epub ahead of print. PMID: 33084377.